Sleep after 45 is a high-leverage “longevity habit“: anchor a consistent simple schedule you can follow, use CBT-I (cognitive behavioral therapy for insomnia) as first-line care, and line up light, caffeine, and screening for sleep apnea so you get restorative nights that power your training and nutrition.
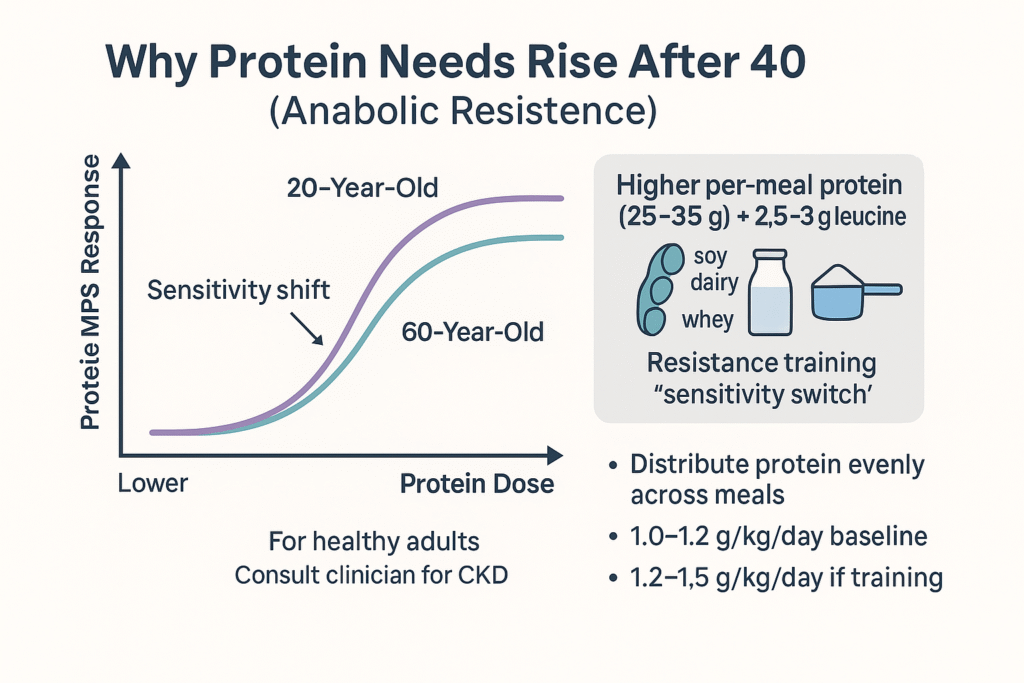
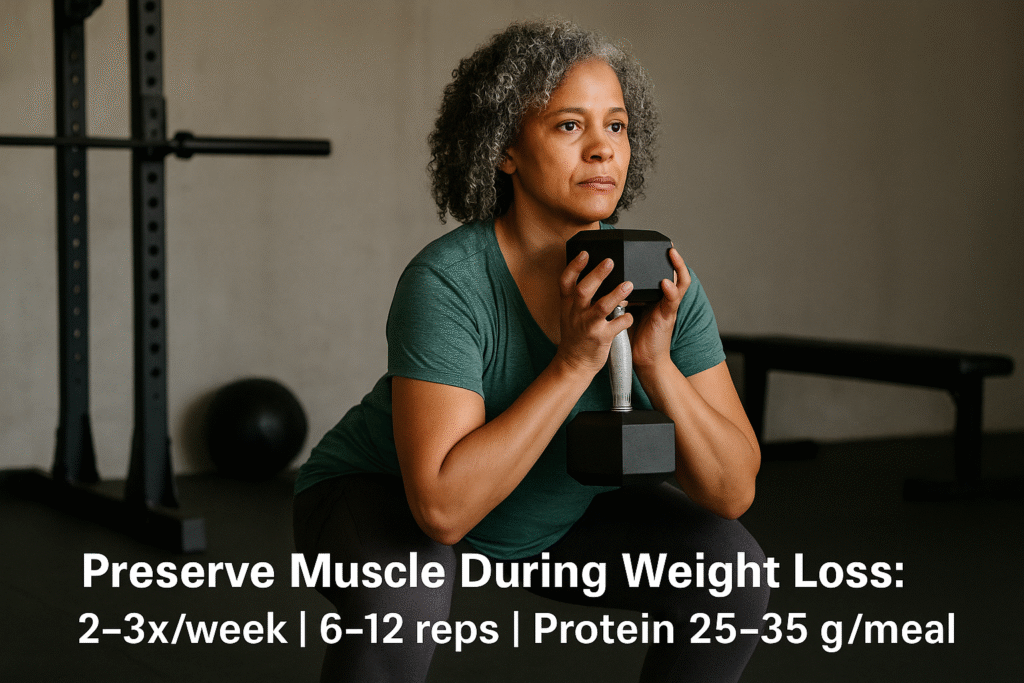
After 45, prioritize CBT-I first for persistent insomnia, morning bright light, no late caffeine (cut off 8–10 hours before bedtime), and OSA (obstructive sleep apnea) screening if you snore or wake unrefreshed. Most adults do best aiming for 7-8 hours (individual needs vary), while CPAP lowers blood pressure when OSA coexists with uncontrolled hypertension. Supplements are an alternative but one should first seek guidance from a medical professional before start a new supplement regimen. Keep the bedroom cool, dark, quiet, and pair great sleep with protein-forward nutrition and two strength days weekly. PubMed+2PMC+2
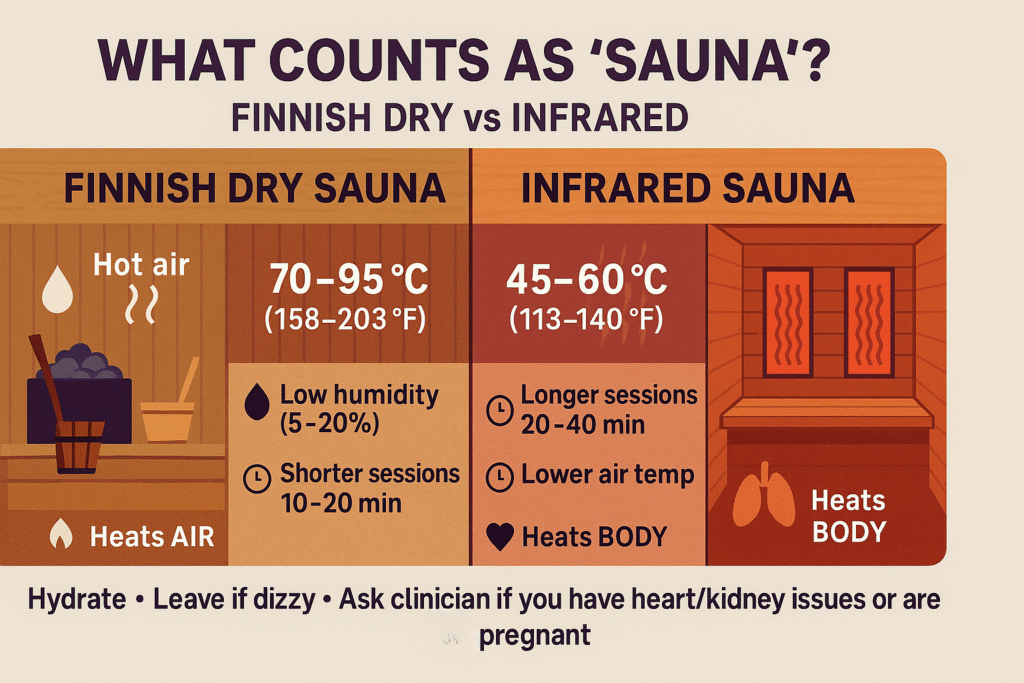
Another tool I find that helps me sleep better is the use of saunas, which has also been found to promote recovery with Heat as a cardiovascular stressor for increasing the heart rate, dilating vessels, and improving skin blood flow. You can read more here: Sauna For Longevity
Why Sleep After 45 Matters for Longevity & Daily Energy

A large body of cohort research shows a U-shaped curve between sleep duration and mortality; both short and long sleep carry higher risk compared with 7-8 hours on average (your best number may differ). Mechanisms run through blood pressure, insulin sensitivity, appetite regulation, immune function, and brain health. Set a consistent ~7-hour sleep opportunity and evaluate by how you feel and function. PMC
Sleep After 45 Starts With CBT-I (Before Pills)
The American Academy of Sleep Medicine (AASM) recommends CBT-I as first-line for chronic insomnia; digital CBT-I tools can help you start if access is limited. The AASM’s pharmacologic guideline suggests against routine melatonin for chronic insomnia in adults (weak, low-certainty evidence). Use medication only in specific, time-limited cases with your clinician. AASM+3PubMed+3AASM+3
CBT-I components (plain English):
Sleep scheduling: Match time-in-bed to actual sleep, then expand as sleep efficiency improves.
Stimulus control: Bed = sleep and intimacy only; if awake 20+ min, get up under dim light and return when sleepy.
Cognitive tools: Defuse catastrophic thoughts about “perfect sleep.”
Wind-down: Predictable, low-arousal routine nightly.
Caffeine Timing: A Big Lever for Sleep Quality
Randomized data show 400 mg caffeine disrupts sleep even when taken six hours before bed; a 2023 meta-analysis found average –45 minutes total sleep time and reduced sleep efficiency with caffeine. Practical rule: stop caffeine 8–10 hours before bedtime (earlier if sensitive), and remember caffeine hides in tea, sodas, energy drinks, and chocolate. JCSM+1
Light: Your Circadian “Reset” for Sleep
Your clock sets with light. To fall asleep earlier and wake refreshed, get outdoor morning light (or a 10,000-lux box) soon after waking; dim indoor lighting at night. Controlled work shows 30 minutes of morning bright light (sometimes with afternoon melatonin in clinical protocols) can phase-advance circadian timing. For most readers, daily AM daylight+ dim evenings is the safest, simplest stack. PMC+1
Don’t Miss Sleep Apnea: A Common Cause of Poor Sleep After 45
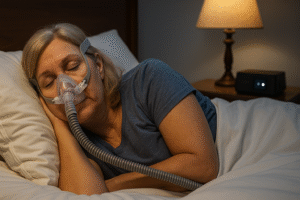
If you snore, feel sleepy, or have hard-to-control blood pressure, screen for OSA. The STOP-Bang questionnaire is a validated tool your clinician can use before ordering a home sleep apnea test or polysomnography. When OSA patients have uncontrolled baseline blood pressure, CPAP therapy yields meaningful BP reductions—an important cardiovascular win. PubMed+1
Avoid Blue Light Before Bed (Behavior Beats Apps)
Evening phone/tablet/laptop exposure suppresses melatonin and delays the clock, making sleep harder; a controlled PNAS study found backlit e-readers before bed reduced melatonin and delayed sleep versus print. The AASM advises a device curfew 30–60 minutes pre-bed; “Night Shift”/warm tints help some, but may not fully prevent melatonin suppression—so lead with behavior: dim lamps, lower light at eye level, and park the phone outside the bedroom. PubMed
Simple Ways to Rebuild Your Sleep Routine
Daily anchors:
Morning light (5–20 min outside) within an hour of waking; evenings dim. PMC
Caffeine cut-off: 8–10 hours before bedtime (longer if sensitive). JCSM
Wind-down: 20–40 minutes of low-arousal habits (stretch, read a paper book, journal).
Bedroom: Cool (~18–20 °C / 65–68 °F), dark, quiet; bed for sleep and intimacy only.
Monday–Sunday sketch:
Mon: AM light + normal day; lights dim 90 minutes pre-bed; fixed bedtime.
Tue: Strength train earlier; finish workouts ≥3–4 hours before bed.
Wed: If exhausted, power nap ≤20 min before 2 p.m.
Thu: Warm shower + wind-down; phone parked outside bedroom.
Fri: Social night? Keep caffeine zero after noon; protect AM light next day.
Weekend: Keep wake time within ~60 minutes of weekdays to avoid “social jet lag.”
Supplements: Complimentary Aides
Magnesium: Evidence in older adults is mixed/low quality; trial modest doses only as an adjunct while you focus on CBT-I, light, and caffeine timing. (Evidence limited—verify for yourself.) AASM
Melatonin: Useful for jet-lag/shift timing when correctly dosed and timed, but AASM suggests against routine use for chronic insomnia in adults. PubMed
Correcting Sleep Issues
3 a.m. awakenings: Lock wake time, push morning light, and enforce the device curfew; apply CBT-I stimulus control (get up under dim light if awake >20 min). PubMed
“I sleep but feel wiped out”: Screen for OSA (STOP-Bang), review meds, and discuss iron/B12 and mood with your clinician. PubMed
Product Picks For Improved Sleep
| Product Image | Product Name / Our Rating / Price | Primary Button |
|---|---|---|
|
Conclusion: Make Sleep After 45 A New Simple Ritual
For midlife and beyond, the winning formula is CBT-I first, morning bright light, early caffeine cut-off, blue-light/device curfew, and OSA screening when symptoms fit—then layer a cool, dark, quiet bedroom on top. Aim for consistent 7-8 hour opportunities, and let better sleep amplify your other pillars—protein-forward meal planning, two strength days, and joint-friendly cardio—so you can lose fat, keep muscle, and feel sharper day to day.
For readers in their late 40s, 50s, and 60s, simplicity = sleep quality. My personal routine: morning light (short outdoor workout or ride in the morning), no caffeine after late afternoon, two strength days, and a boring wind-down (stretch, paper book, lights low). If I’m waking unrefreshed, I screen for apnea rather than pile on supplements. I treat gadgets as helpers (light box, blackout curtains) and CBT-I as the foundation when insomnia creeps in. The goal isn’t perfect sleep every night—it’s more predictable, restorative weeks that make training, nutrition, and mood easier.
Disclaimer: All the content on this site is for informational purposes only, does not constitute medical advice, and does not establish any kind of patient-client relationship by your use of this website. I am not a health care professional. The information, including but not limited to text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis, or treatment. Before starting any new regimen, supplement, diet, or program, it is crucial to consult with a healthcare professional to ensure it is safe and suitable for your individual health needs and circumstances. Here’s a little transparency: This website also contains affiliate links. This means if you click and make a purchase, we may receive a small commission. Don’t worry, there’s no extra cost to you. It’s a simple way you can support our mission to bring you quality content.